No one goes into medicine to cause harm. Doctors, nurses, techs, administrators, PAs, CNAs, and all other staff come together to bring life and give hope. Hospitals should be places of healing – not new illnesses. But for many patients, that’s the unfortunate reality. Hospital Acquired Infections (HAIs) present threats to patients, staff, and the hospital itself. Determining the source of infections and reducing the spread of infections in hospitals should be a high priority, but it goes beyond sterilization, PPE quality, and hand washing procedures.
Like most things in the healthcare field, reducing the spread of infections is complicated, because infectious germs are complicated. But it does come down to one seemingly simple principle: cleanliness. Currently best practices and protocols focus heavily on instrument, personnel, and surface cleanliness. But what about the air?
What Are HAIs?
Before we can get into how filtration can help, we first need to understand exactly what HAIs are. When most people think of HAIs, they think of Central Line-associated Bloodstream Infection (CLABSI), Catheter-associated Urinary Tract Infections (CAUTI), Surgical Site Infection (SSI), and Ventilator-associated Pneumonia (VAP). Best practices for avoiding these involve personnel hand hygiene, maintaining sterile fields, and other traditional practices, but those practices don’t prevent infectious particles that travel through the air on droplets.
In the last few years, we’ve heard a lot about how viruses, like COVID-19, travel certain distances on the droplets we exhale, but in a hospital setting, there are numerous other kinds of infections and diseases to consider. Tuberculosis, norovirus, and even MRSA, among other potential threats, can all travel on droplets and cause serious, life-threatening infections and illnesses for hospital patients.
The CDC estimates there are over 1.7 million HAIs every year, resulting in 99,000 deaths. While the toll on people’s healths and lives is enough to drive action, HAIs also exact a fiscal toll. Every year, HAIs directly cost hospitals over $28.4 billion in the US. So what else can hospitals do to make a difference?
How Can Air Filtration Help Reduce the Spread of Illness in Hospitals?
Air filtration, when done right, can provide a powerful barrier that pulls these microscopic particles from the air, protecting both patients and hospital staff. Air filtration should be integrated into the HVAC system, with concentrations of filters around high risk rooms, such as quarantine units and ICUs.
Most Penetrating Particle Size (MPPS)
Before we can jump into the types of filters available and how they can help your hospital, we need to understand a very functional part of filters: the most penetrating particle size (MPPS) of each filter. This concept is slightly counterintuitive, but it makes sense in the end.
The MPPS is the diameter of the particle which will most easily pass through the filter. This makes sense, right? But this is where it gets tricky: particles that are both larger and smaller than the MPPS have a more difficult time passing through the filter. This means a filter might be more effective at preventing smaller particles from passing through than the MPPS.
Essentially, this makes the MPPS the worst case scenario. The efficiency rate is improved for both larger and smaller particles until a defined size of smaller particle.
Types Of Filters
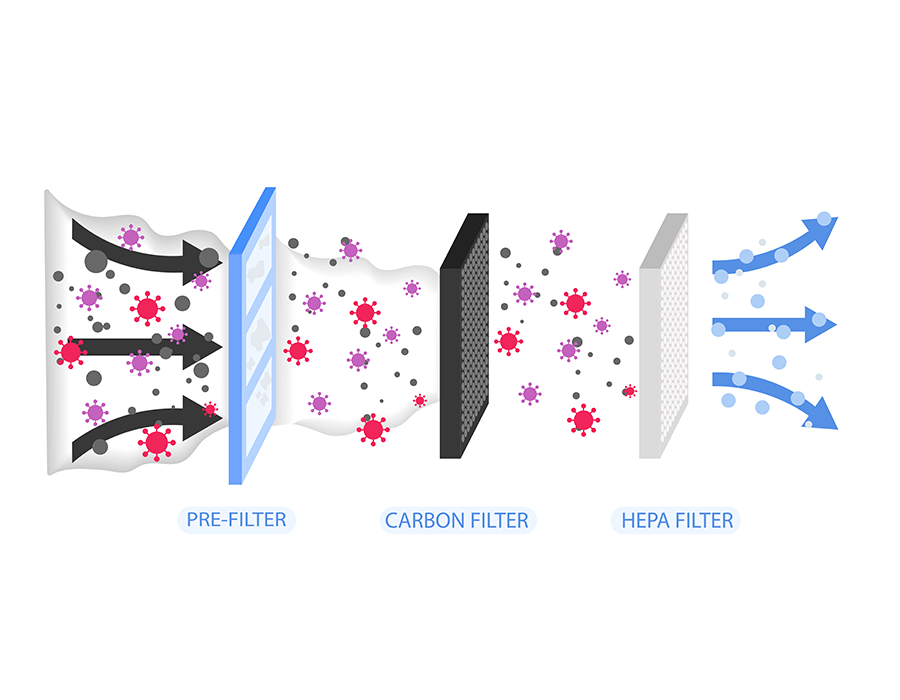
There are a number of types of filters that you can integrate into your HVAC system and they each play a different role. Most HVAC systems that filter air use a combination of several types of filters to capture the most particles possible.
Pre-Filters
Pre-filters are the frontline of filters. They have thicker fibers and catch large particles before the air flows through the finer filters, such as HEPA and ULPA filters. Because they bear the brunt of bulk filtration, they should be replaced roughly 6 times a year. They are cheaper to replace than ULPA or HEPA filters and they prolong the lives of your more expensive and sensitive filters.
Activated Charcoal Filters
Activated charcoal filters serve a unique purpose: they are highly porous filters designed to absorb fumes. They are very effective at absorbing fumes in negative pressure environments, which is a common technology used in quarantine units.
Lingering smells can cause unease and decrease productivity and comfort. Integrating charcoal filters can help ease this burden. Their replacement timeline depends on the intensity of use.
HEPA Filters
Now we have made our way to the most sensitive filters: HEPA and ULPA filters. High Efficiency Particulate Air (HEPA) filters are more common than ULPA filters. According to the Environmental Protection Agency (EPA), they are “a type of pleated mechanical air filter”. HEPA filters have an MPPS of 0.3 microns at a rate of 99.97% efficiency. For reference, MRSA particles range from 7 to 12 microns in size, making HEPA filters highly effective. But COVID-19 virus particles can be as small as 0.1 microns in size.
HEPA filters have a relatively long life, if taken care of well. They should be replaced every 4 to 6 years, depending on the application.
ULPA Filters
If you’re looking for ultimate protection, Ultra Low Particulate Air (ULPA) filters are the next most efficient. They have an MPPS of 1.2 microns with a removal efficiency of 99.9995% for the MPPS, but they specialize in capturing smaller particles, down .12 microns. Thus, they are more apt for specialized applications.
ULPA filters can also last several years but do need to be replaced after a few years, depending on your application and other filtration systems in place.
Implementing Air Filtration to Reduce The Spread of Infections in Hospitals
Using air filtration, specifically HEPA filters, is an engineering method of reducing the spread of these infectious particles in a hospital. Research shows that these types of methods can help reduce the risk for staff and patients.
While a potentially costly endeavor, implementing and maintaining an air filtration strategy can literally save lives, as well as billions of dollars in addressing HAIs.
But at the end of the day, if you want to know exactly what’s going on in your hospital’s air… That’s a different story.
Check out our Knowledge Center to learn more!